Prostate cancer, a common but often indolent disease, presents a unique challenge for early detection. While early diagnosis can prevent the progression of aggressive cancers, a large percentage of prostate cancers are slow-growing, meaning they might never cause harm during a man’s lifetime. Treating these non-lethal cancers can result in unnecessary surgeries, radiation, and their side effects, which include impaired sexual function and urinary health. For years, the medical community has debated how to balance the benefits of early detection with the risks of overdiagnosis and overtreatment.
The recent introduction of Magnetic Resonance Imaging (MRI) as part of the screening process for prostate cancer has opened a new chapter in addressing these concerns. A groundbreaking study published in the New England Journal of Medicine shows that incorporating MRIs can reduce unnecessary prostate cancer diagnoses and treatments by more than half. This discovery is shifting perspectives on how prostate cancer screening should be conducted, potentially offering a solution to the dilemma of overdiagnosis.
The Problem with Traditional Screening: PSA Testing
Prostate cancer screening traditionally relies on the Prostate-Specific Antigen (PSA) test. The PSA test measures the level of PSA, a protein produced by the prostate, in a man’s blood. Elevated PSA levels can indicate the presence of prostate cancer, but they can also be caused by benign conditions such as prostatitis or benign prostatic hyperplasia (BPH). Because of its lack of specificity, the PSA test often leads to the detection of low-grade, slow-growing cancers that may never cause harm—also known as indolent cancers.
The treatment of these indolent cancers often involves surgery or radiation, which comes with significant side effects such as incontinence and erectile dysfunction. Over the years, this led to concerns that PSA testing might do more harm than good. In fact, large-scale clinical trials in the late 2000s found that PSA testing resulted in only modest reductions in mortality. As a result, many experts became skeptical of the test’s benefits, recommending that patients make shared decisions with their doctors about whether or not to undergo screening.
The Shift Towards MRI in Screening
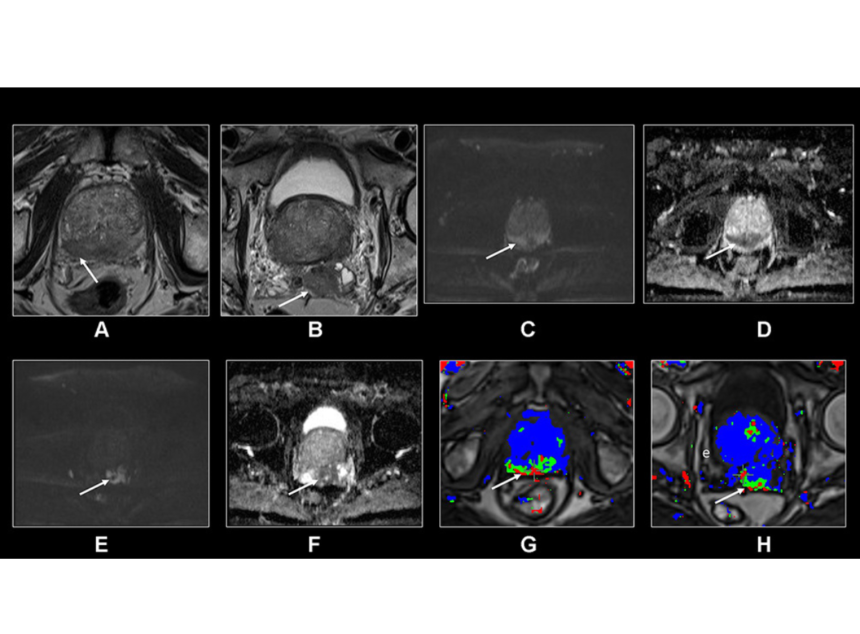
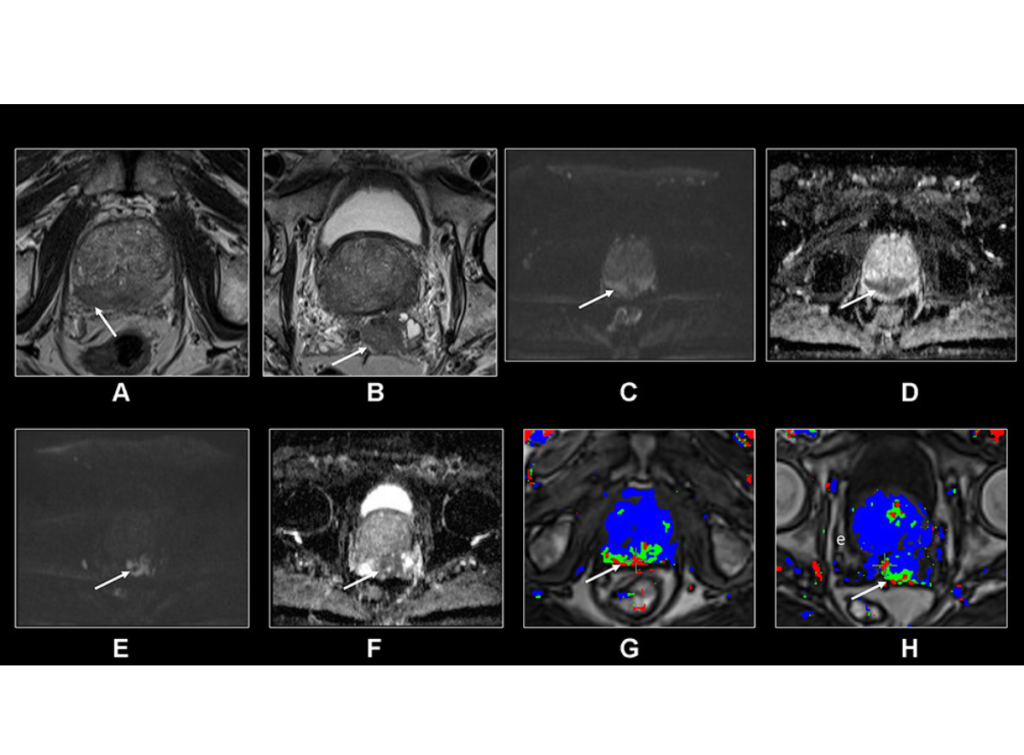
To mitigate the risks of overdiagnosis and overtreatment, researchers have been looking for ways to make prostate cancer screening smarter and more targeted. The latest innovation is the use of MRI scans to guide biopsies and determine which patients actually need treatment. This new strategy could mark a significant improvement over traditional methods.
A large study conducted by Jonas Hugosson, a professor of urology at the University of Gothenburg in Sweden, has provided the strongest evidence to date that MRI-guided screening reduces unnecessary biopsies and overdiagnosis. The study enrolled approximately 13,000 men in Sweden and followed a two-step screening process:
- Men with elevated PSA levels (above 3 nanograms per milliliter of blood) received an MRI scan.
- Based on the MRI results, only men with suspicious lesions underwent a targeted biopsy. In contrast, the control group received both a targeted biopsy (if a lesion was present) and a systematic biopsy, where samples are taken from all parts of the prostate.
Results: Fewer Biopsies, Reduced Overdiagnosis
The results of the study were promising. Among men who only received biopsies if a lesion appeared on their MRI, the frequency of biopsies was reduced by about 60%, and the rate of overdiagnosis dropped by approximately 57%. This is a significant reduction in both the number of unnecessary procedures and the diagnosis of indolent cancers that likely would never have caused harm.
Furthermore, the study showed that this more selective approach did not result in a statistically significant increase in missed aggressive cancers. Only a few men in the targeted biopsy group went on to develop clinically significant cancers that had not been detected in the initial screening, and these cancers were caught on subsequent tests. This suggests that delaying the biopsy in men without MRI-detected lesions is a safe strategy that spares many men from unnecessary treatment.
Reducing Overdiagnosis: A Safer, More Efficient Approach
The significance of these findings is clear: MRI-guided screening can reduce the harms associated with prostate cancer diagnosis, including the emotional and physical toll of unnecessary treatments.
The traditional approach, where biopsies are conducted based solely on elevated PSA levels, often leads to the discovery of low-grade cancers that would never have become life-threatening. These men are then subjected to invasive treatments that can dramatically impact their quality of life. In contrast, the MRI-targeted approach reduces the number of unnecessary procedures and focuses on finding aggressive, clinically significant cancers.
Moreover, by using MRI to detect suspicious lesions, doctors can avoid systematic biopsies, which are more invasive and carry a higher risk of side effects like infection and bleeding. Instead, they can take targeted samples only from areas of the prostate that appear abnormal on the scan.
Challenges: MRI Accessibility and Infrastructure
While the results of Hugosson’s study are encouraging, there are significant barriers to implementing MRI-guided screening on a large scale. For one, the availability of MRI machines and the expertise needed to interpret the scans are limited, particularly in rural areas. In many regions, there simply aren’t enough MRI scanners or specialized radiologists to make this approach feasible.
In urban areas, where medical infrastructure is more robust, only about a third of men currently receive an MRI before undergoing a prostate biopsy. Expanding MRI use for prostate cancer screening would require substantial investment in both equipment and training. Tyler Seibert, a radiation oncologist and prostate cancer researcher at the University of California, San Diego, noted that MRI scans of the prostate are complex and require a high degree of expertise to perform and interpret correctly.
The Future: Improving Prostate Screening with Technology
Despite the challenges, researchers are optimistic about the future of MRI-guided prostate cancer screening. Seibert and others are working on solutions to improve the accessibility of this technology, such as developing AI tools that can help interpret MRI results and making the scanning process more standardized and efficient. By automating parts of the diagnostic process, they hope to reduce the reliance on specialized radiologists and increase the availability of MRI for prostate screening.
In addition to MRI, scientists are also exploring other ways to make prostate cancer screening more precise. This includes the development of new blood and urine biomarkers that could complement or even replace the PSA test, as well as personalized screening programs that take into account an individual’s genetic risk for prostate cancer.
Conclusion: A New Era for Prostate Cancer Screening
The integration of MRI into prostate cancer screening represents a significant advance in the effort to balance the benefits of early detection with the risks of overdiagnosis. While challenges remain in terms of infrastructure and accessibility, the evidence suggests that MRI-guided biopsies can significantly reduce unnecessary procedures and improve patient outcomes.
For men considering prostate cancer screening, this approach may offer a safer and more efficient way to detect aggressive cancers while avoiding the harms of overtreatment. As technology continues to improve, MRI could become a cornerstone of prostate cancer screening, helping to save lives and reduce the burden of unnecessary treatments.